Clinical Gems - Foot and Ankle
Claire offers expert advice for the not so typical spained ankle
The foot and ankle are integral to human movement, expertly balancing stability to support the body, mobility to adapt and move efficiently, and propulsion to drive us forward in both every day and athletic activities. Poorly rehabilitated injuries can lead to a cascade of both local pain whole body deconditioning.
While most ankle injuries involve the lateral ligaments due to inversion, others—such as syndesmosis (high ankle) injuries, sinus tarsi syndrome, cuboid injuries, and midfoot sprains—present with different mechanisms, symptoms, and management needs. Recognising these distinctions helps prevent missed diagnoses and long-term complications.

Syndesmosis injuries
These often occur with ankle external rotation while in dorsiflexion (as opposed to plantarflexion inversion injuries). Pain is located above the talus. The usually require imaging. Note, don’t forget to get full length fibular views due to associated spiral fractures and unstable injuries can need surgical fixation. Missed injuries often lead to chronic instability and arthritis.
Clinical Gem - For low grade sprains a simple tennis elbow band to bind the tib and fib together and provide instant relief weight bearing and guide rehabilitation.

Tibialis posterior tendon injury
ibialis Posterior tendon injury commonly results in pain at two sites the navicular and about the medial malleoli. It’s unique role is to also stabilise the foot in the frontal plane. With acute injury it is imperative that support is provided also in this plane. Poor rehabilitation of this can lead to an acquired flat foot or sinus tarsi syndrome.
Clinical gem – A dynamic tape to lift the navicular or a medial heel wedge +/- arch support do wonders in the short term for these injuries. High load strengthening is then a necessity for management.
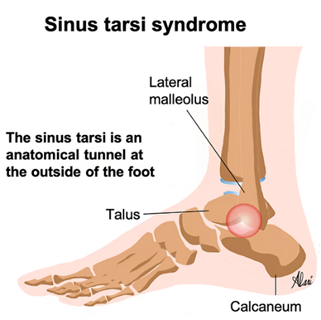
Sinus Tarsi Syndrome
·Pain localized to the lateral hindfoot and the patient may have a tendence to a flat foot or have had repeated sprains and instability.
·Clinical Gem: These injuries often settle well with a supportive heel lock taping to hold in subtalar neutral during the acute inflammatory phase and strengthening the mid foot for longer term rehabilitation.
Cuboid Sprains
·Lateral midfoot pain, sometimes with subtle subluxation or fracture; may be misdiagnosed as a simple sprain. Common in athletes such as gymnasts and dances who have an inversion injury while in demi pointe. Gait and ankle joint movements are often full and pain free here but rotation of the mid foot reproduces pain. The patient also complains of pain rising onto toes.
Clinical Gem: Manipulation or mobilisation of the cuboid can often relieve pain but this should be followed up with stabilisation using a rigid basket weave about the midfoot and intrinsic foot strength are imperative for sustainable management.

Not to be forgotten... Chopart and Lisfranc injuries
The Chopart joint complex, also known as the midtarsal or transverse tarsal joint and injury involves two main joints: the talonavicular and calcaneocuboid. A Lisfranc injury refers to damage involving the midfoot, specifically at the tarsometatarsal (TMT) joints.
Complete disruption of these joints often results from high-energy trauma such as motor vehicle accidents, falls from height, or severe twisting injuries. Direct trauma such as a heavy object falling on the foot is also a common cause for a Lisfranc injury.
Complete disruption of these joints often results from high-energy trauma such as motor vehicle accidents, falls from height, or severe twisting injuries. Direct trauma such as a heavy object falling on the foot is also a common cause for a Lisfranc injury.
Injuries to both of these joints typically need imaging. Injury may require surgical intervention to restore anatomical alignment and stability, often using internal fixation or, in some cases, primary arthrodesis (fusion) of the affect ted joints. Stable non displaced injuries maybe often managed non- weight bearing for up to 6 weeks.

How long do foot and ankle injuries take to get better? When can I play again?
These are golden questions so often asked. As well as clinical symptoms and sport specific demands on the foot I use a progressive loading approach to all foot and ankle injuries.
I use a combination of the acute /chronic work load for sustainability, muscle strength and power measurements using VALD dynamometry and dynamic lateral hop to check reactive stability to allow guidance for return to play in a safe and sustainable way.
I continue to prioritize the both the youth acute lower limb assessment and the complex foot and ankle in my acute triage appointments so that we can keep our community active and mitigate recurrent injury.